Type 2 Diabetes Stem Cell Therapy: A New Chapter in Managing Blood Sugar
Living with type 2 diabetes is exhausting. The daily finger-pricks, the constant monitoring of what you eat, the worry about long-term complications — it wears people down over time. That’s why so many patients and researchers alike have been holding their breath as a promising frontier quietly gains momentum: type 2 diabetes stem cell therapy. This isn’t science fiction anymore. It’s a rapidly evolving field that’s beginning to offer real hope — not just for better management, but potentially for something people have been told was impossible: a lasting solution.
Understanding the Root Problem
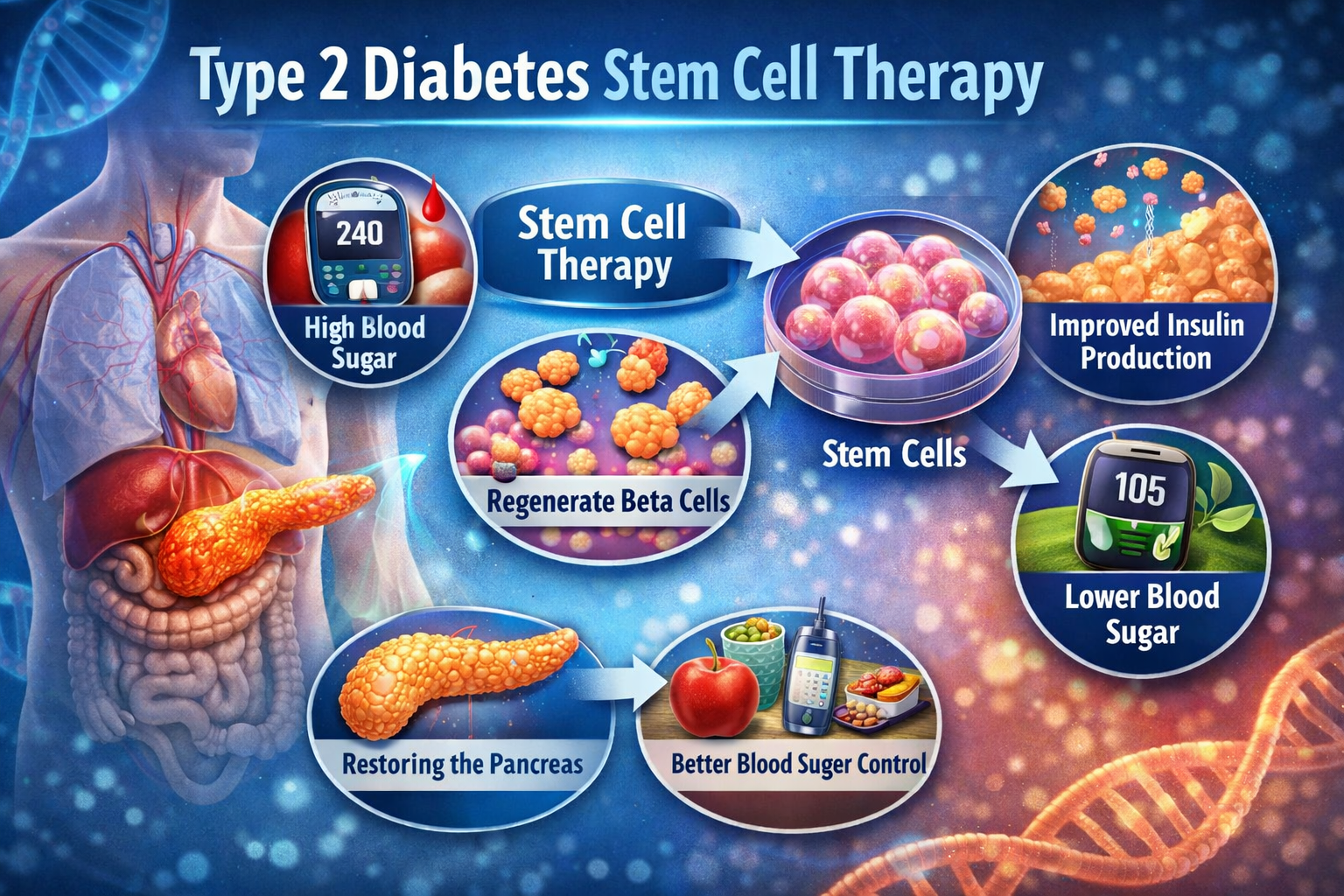
To understand why stem cell therapy is generating so much excitement, it helps to revisit what’s actually going wrong in the body. In type 2 diabetes, two things break down simultaneously: the cells in your muscles and liver stop responding properly to insulin, and the beta cells in your pancreas — the ones responsible for producing that insulin — gradually burn out from the overwork. Most current treatments address the symptoms, adjusting blood sugar levels through medication or lifestyle changes. But they don’t repair the underlying damage. That’s where stem cells enter the picture.
What Stem Cell Therapy Actually Does
Stem cells are essentially the body’s raw material — undifferentiated cells that have the remarkable ability to become many different types of cells. In the context of type 2 diabetes stem cell therapy, researchers are pursuing several approaches at once. Some teams are working on coaxing stem cells to become functional, insulin-producing beta cells that can be transplanted into the pancreas. Others are focusing on mesenchymal stem cells, which seem to reduce inflammation and improve insulin sensitivity throughout the body. Still others are exploring how stem cells might help repair the small blood vessels damaged by years of high blood sugar — damage that leads to complications in the kidneys, eyes, and nerves.
What the Research Is Telling Us
The clinical trial landscape for type 2 diabetes stem cell therapy has grown significantly over the last decade. Early-phase trials have shown that some patients experience meaningful reductions in their need for insulin after treatment. In several studies involving mesenchymal stem cells — often sourced from umbilical cord tissue or the patient’s own bone marrow — participants saw improvements in fasting blood glucose and HbA1c levels, sometimes for months after just a single infusion. One particularly encouraging line of research involves encapsulated beta cells derived from stem cells, which can produce insulin in response to blood sugar changes while being shielded from immune attack. While these results are still considered preliminary, the consistency across multiple studies is hard to dismiss.
The Challenges That Remain
Honest enthusiasm means acknowledging the hurdles too. Type 2 diabetes stem cell therapy still faces significant questions around safety, durability, and accessibility. The immune system can attack transplanted cells, which is why researchers are working hard on techniques to protect them. The effects seen in trials have sometimes faded over time, raising questions about how long benefits actually last. And the cost and complexity of these procedures, at least in their current form, would put them out of reach for most patients if they were approved tomorrow. Regulatory pathways are also lengthy, and for good reason — ensuring something is genuinely safe and effective takes time.
Why This Matters for Real Patients
It’s easy to get lost in the science and forget the human dimension. There are over 500 million people living with diabetes worldwide, and the vast majority have type 2. For many, the disease progresses despite their best efforts — tighter control, more medication, further lifestyle changes. The psychological burden of a condition that feels relentless is real and often underappreciated. The potential of type 2 diabetes stem cell therapy isn’t just clinical; it’s deeply personal. Even a treatment that could meaningfully reduce insulin dependence, slow progression, or lower the risk of complications would change millions of lives.
Looking Ahead With Realistic Optimism
Major biotech companies and academic medical centers are now investing heavily in this area. Several late-phase trials are underway, and some observers believe that a commercially available stem cell-based treatment for type 2 diabetes could be a reality within the next decade. The science is moving faster than most people realize. That said, anyone currently living with type 2 diabetes should approach claims about unregulated stem cell clinics with real caution — not every offering marketed as type 2 diabetes stem cell therapy meets rigorous scientific standards, and some carry genuine risks.
Final Thoughts
The story of type 2 diabetes has long been one of management rather than resolution. But that story may be changing. Stem cell research is quietly rewriting what we think is possible — not with dramatic announcements, but with careful, incremental progress. For patients who have spent years adjusting to a condition that medicine said could only be controlled, not cured, that progress is worth watching closely. The road ahead still has twists in it. But for the first time in a long time, it seems to be heading somewhere genuinely new.